Blood Supply
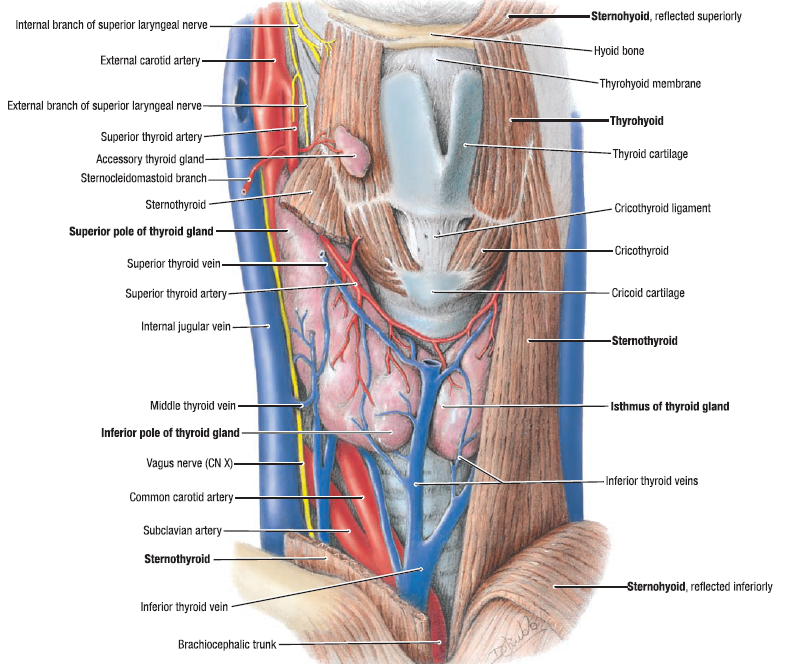
The superior pole of the gland is supplied by multiple branches of the superior thyroid artery as it originates from the external carotid artery.
During thyroidectomy great care must be taken to expose the avascular space between the cricothyroid muscle and the superior pole of the gland. The branches of the superior thyroid artery should be ligated as close to the gland as possible to prevent inadvertent incorporation of the external branch of the superior laryngeal nerve.
This nerve often runs in a similar path with the superior thyroid artery; its anatomic variations are well described by Cernea et al.4
In addition to exposing the avascular cricothyroid space, the lateral aspect of the superior pole needs to be dissected free of the overlying sternothyroid muscle. Inferolateral traction on the gland is crucial in exposing both of these planes of dissection to safely ligate the superior pole.
The inferior thyroid artery arises from the thyrocervical trunk and gives off terminal branches entering the posterolateral aspect of the thyroid at the junction of the upper and middle third of the gland. It is intimately associated with the recurrent laryngeal nerve and runs along a course that generally intersects the nerve as its branches terminate in the gland.
Venous Drainage
Venous drainage of the thyroid gland is variable and occurs through a variety of intercommunicating vessels. The venous network may be divided into three separate regions: the superior veins (draining the superior pole and adjacent to the superior thyroid arteries); the middle thyroid veins (which may be absent in some patients), traveling laterally from each lobe and emptying into the internal jugular vein; and the inferior thyroid veins, draining the inferior pole and adjacent to and coursing with the thyrothymic ligament.
Nerves
Three major components of the nervous system are encountered in thyroid surgery. At the superior pole of the thyroid is the external branch of the superior laryngeal nerve (EBSLN). It is a branch of the vagus nerve and is the motor nerve supplying the cricothyroid muscle. As previously noted, its close but variable course to the superior pole vessels place it at risk for injury during thyroidectomy.4 When effort is taken to identify it as it courses through the cricothyroid space, the nerve may be found in more than 90% of cases.
The recurrent laryngeal nerves (RLNs) ascend from the thoracic inlet along the right and left tracheoesophageal grooves. Compared with the nerve on the left, the nerve on the right courses in a more lateral to medial oblique path. The nerves may give off anterior or posterior branches before entering the larynx. There are many variations of the nerve and its relation to the ligament of Berry as well as the inferior thyroid artery; however, it can generally be encountered passing into the pharynx in a cleft just medial to the tubercle of Zuckerkandl.1 A nonrecurrent laryngeal nerve is rare (<1%); if present, it is usually found on the right. Left-sided nonrecurrent laryngeal nerves are extremely uncommon, although a recent case report noted a patient with a right aortic arch, an aberrant left innominate artery, and the absence of a ductus arteriosus.5 A nonrecurrent nerve tracks along the same course as the vagus and sweeps from lateral to medial in the jugulocarotid groove. It is most commonly associated with a retroesophageal aberrant subclavian artery (lusorian artery).
An additional set of nerves that deserves mention are the sympathetic–inferior laryngeal nerve anastomotic branch (SILABs), which run between the cervical sympathetic ganglia and the recurrent laryngeal nerve with fine direct anastomosis and then run onto the surface of the gland itself. The SILAB may be larger than the RLN and as such leads to confusion in identification of the RLN, thus placing it at risk for injury. SILABs may be divided with impunity during capsular dissection, but their visualization is necessary to ensure proper identification and preservation of the RLN.1
The thyroid gland is highly vascularized with arterial blood derived from the superior and inferior thyroid arteries. The veins draining the thyroid gland form a plexus on the surface of the gland and on the front of the trachea and give rise to the superior, middle, and inferior thyroid veins, which drain into the internal jugular and innominate veins. The lymphatic vessels end in the thoracic and right lymphatic trunks. Innervation to the thyroid gland is provided through the middle and inferior cervical ganglia of the sympathetic nervous system.